Gut microbes may predict the effectiveness of anthelminthic drugs
Pre-screening of the gut microbiome may lead to a more personalized approach to treating intestinal parasitic worm infections, leading to better treatment outcomes and a decreased risk for drug resistance.
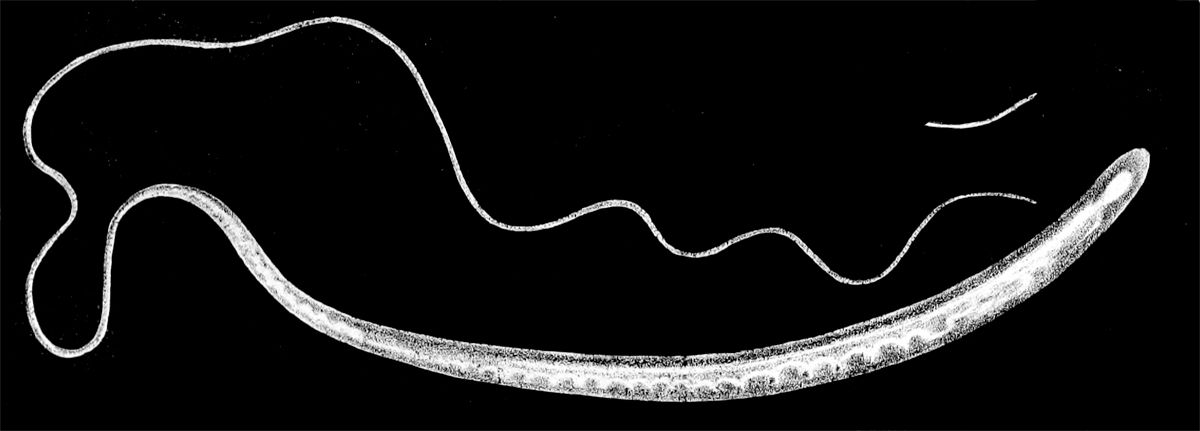
If the microbes in human intestines hosted a formal gathering, parasitic worms would be the party crashers. Upsetting the status quo to burrow through intestinal walls and lay their eggs, these worms make themselves at home where the bacteria, viruses, and archaea of the gut microbiome already live.
The problem is that when drugs reach the intestines to throw out these parasitic trespassers, the gut microbes already at the soirée may determine how well the treatment works.
In a new Nature Communications study, researchers at the Swiss Tropical and Public Health Institute reported that certain communities of gut bacteria in people infected with hookworms and whipworms predicted how well they responded to anthelminthic treatment (1). Understanding how the gut microbiome interacts with antiparasitic drugs could lead to a more effective and targeted approach to drug administration, reducing the administration of ineffective treatments that promote the rise of drug resistance.
“The interaction between treatment and microbiome [is] an interesting perspective that I don't think is very much studied,” said Nolwenn Dheilly, a parasitologist at the French Agency for Food, Environmental and Occupational Health & Safety (ANSES) who was not involved in the study. This new research “reveals a gap in knowledge that would also apply to other diseases.”
For years, the standard of care for most parasitic worm infections has been either one of two benzimidazole-based drugs: albendazole or mebendazole, but for certain species of parasitic worms such as Trichuris trichiura, a whipworm, these drugs are not very effective. Instead, researchers have found that the combination therapy of albendazole and ivermectin works better against multiple species of parasitic worms, including hookworms, roundworms, and whipworms. While this combination therapy has improved cure rates overall, Pierre Schneeberger, a microbiome researcher at Swiss Tropical and Public Health Institute and the lead author of the new study, and his team demonstrated that its effectiveness varies vastly across populations, from a 14% cure rate for T. trichiura infections in Côte d'Ivoire to 66% in Laos (2).
“Why do we see so much failure? Why do we see so many differences between patients?” Schneeberger asked.
Because human parasitic worms set up shop in the intestines — hookworms and roundworms in the small intestine and whipworms at the start of the large intestine — Schneeberger and his colleagues hypothesized that the resident gut microbes influenced the effectiveness of the albendazole and ivermectin treatment.
To investigate this hypothesis, Schneenerger and his team collected stool samples from people across 10 villages in Laos who were infected with both hookworms and T. trichiura.

Ensuring that patients placed their stool samples in a refrigerator or freezer as soon as they collected it was one of the most challenging aspects of this study, Schneeberger said. Although scientists often downplay the fieldwork aspects of their research, proper storage of these samples in resource constrained countries can be incredibly difficult. If stool samples are left out of a freezer too long, Schneeberger explained, “you have further bacterial growth, which might, in the end, change or bias the communities that you're actually investigating.”
Once the research team collected patient stool samples, they gave 41 patients albendazole treatment and 39 patients the albendazole plus ivermectin combination therapy.
Schneeberger’s team then analyzed the patient’s pre-treatment gut microbiomes. Using several bacterial sequencing approaches combined with unsupervised clustering, the researchers classified patients into one of three different groups, called enterotypes (ET1, ET2, and ET3), based on the similarity of their gut microbiomes.
For patients only treated with albendazole, there was no association between enterotype and cure rate. However, for the patients who received the combination albendazole and ivermectin treatment, the majority who were cured fell into the ET3 group. Schneeberger’s team also found that patients in the ET3 group were cured faster than those in the ET1 or ET2 group who had received the same combination treatment.
“The strength of the association with treatment outcomes surprised me,” said Schneeberger. “Such a strong association is usually difficult to get in microbiome research.”
To investigate why patients with ET3 had a better treatment outcome, Schneeberger and his team profiled the metabolic pathways enriched in each enterotype. They found that ET1 and ET2 were enriched for metabolic pathways known to support helminth infection, suggesting that the gut microbiome may make it easier for parasites to colonize the intestines of these patients. But how exactly the gut microbes in ET3 contribute to better cure rates and why ET1 and ET2 associate with poorer outcomes will require additional research.
Yvonne Ai Lian Lim, a parasitologist and gut microbiome research at Universiti Malaya who was not involved in the study, was impressed with the robustness of the researchers’ analyses, but she cautioned that with the study’s low sample size and limited geographic location, the results cannot be generalized to a larger population without further research.
Schneeberger agrees, and he and his team are working on addressing these points in an ongoing validation study in Laos with more participants and in additional studies taking place in Western and Eastern Africa.
“There is such diversity in the gut microbiome that maybe one taxon that is associated with failure of treatment in Laos might be another species or another taxon in Ivory Coast. And of course, that's why it would be very interesting to understand the mechanisms at play,” said Schneeberger.
In addition to producing metabolic products that make the gut more hospitable to parasitic worms, gut microbes could also directly interact with anthelminthic drugs, Schneeberger hypothesized. Anthelmintic drugs can have antibacterial properties, so it’s possible that certain species of bacteria evolve resistance to the drug and inactivate or sequester it, thus preventing the treatment from killing the parasites.
Schneeberger hopes that a better understanding of the mechanisms involved in the interactions between the gut microbiome and anthelminthic treatment will enable clinicians to move away from mass drug administration and target therapies to the people who will benefit from them the most.
“We could potentially come up with a pre-screening tool that is much cheaper that can also be conducted on site directly before we actually give the anthelminthic treatment,” Schneeberger said. “We need to dig a little bit more into the pharmaco-microbiome interactions of these massively used drugs and understand what they actually do to the microbiome or how they interact.”
References
- Schneeberger, P.H.H. et al. Different gut microbial communities correlate with efficacy of albendazole-ivermectin against soil-transmitted helminthiases. Nat Commun 13, 1063 (2022).
- Hürlimann, E. et al. Efficacy and safety of co-administered ivermectin and albendazole in school-aged children and adults infected with Trichuris trichiura in Côte d'Ivoire, Laos, and Pemba Island, Tanzania: a double-blind, parallel-group, phase 3, randomised controlled trial. The Lancet Infectious Diseases 22, 123-135 (2022).




