Learning new techniques against lymphomas
Researchers have published on a new CAR-T cell therapy using CXCR5
BERLIN—Researchers from the Max Delbrück Center for Molecular Medicine (MDC), which is part of the Helmholtz Association, have developed a new approach to CAR T cell therapy. The study, published in Nature Communications, has shown that the procedure is very effective — particularly for fighting follicular lymphomas and chronic lymphocytic leukemia.
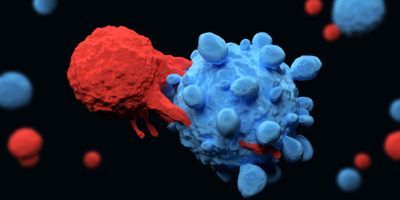
Until now, Chimeric antigen receptor (CAR) T cells have been primarily directed against the protein CD19, which B cells carry on their surface. A team led by Dr. Uta Höpken has now developed a new twist on this therapy that sensitizes the T cells in the laboratory to a different identifying feature: the B-cell homing protein CXCR5.
“CXCR5 was first described at the MDC more than 20 years ago, and I have been studying this protein myself for almost as long,” explained Höpken, who is head of the Microenvironmental Regulation in Autoimmunity and Cancer Lab at the MDC, and corresponding author for the study. “I am therefore very pleased that we have now succeeded in using CXCR5 to effectively combat non-Hodgkin’s lymphomas such as follicular and mantle cell lymphoma, as well as chronic lymphocytic leukemias, in the laboratory.”
CXCR5 is a receptor that helps mature B cells move from bone marrow to immune system organs, like the lymph nodes and spleen.
“All mature B cells, including malignant ones, carry this receptor on their surface. So it seemed to us to be well suited to detect B-cell tumors — thereby enabling CAR-T cells directed against CXCR5 to attack the cancer. In our study, we have shown through experiments with human cancer cells and two mouse models that this immunotherapy is most likely safe and very effective,” added Janina Pfeilschifter, a PhD student in Höpken’s team, and a lead author of the study.
The new approach could be particularly well suited for patients with a follicular lymphoma or chronic lymphocytic leukemia (CLL).
“Both types of cancer involve not only B cells but also follicular T helper cells, which also carry CXCR5 on their surface,” noted Dr. Mario Bunse, also a lead author.
The CXCR5-CAR was generated by Dr. Julia Bluhm when she was a PhD student in the MDC’s Translational Tumorimmunology Lab headed by Dr. Armin Rehm, who is also a corresponding author of the study.
Pfeilschifter and Bunse first showed that various human cells — like those from blood vessels, the gut, and the brain — don’t carry the CXCR5 receptor on their surface, and therefore aren’t attacked in the petri dish by T cells equipped with CXCR5-CAR.
“This is important to prevent unexpected organ damage from occurring during therapy,” pointed out Pfeilschifter.
Experiments with human tumor cell lines showed that malignant B cells from very different forms of B-non-Hodgkin’s lymphoma all display the CXCR5 receptor.
Professor Joerg Westermann, in the Division of Hematology, Oncology, and Tumor Immunology for the medical department of Charite - Universitaetsmedizin Berlin at the Campus Virchow Clinic, also provided the team with tumor cells from patients with CLL or B-non-Hodgkin’s lymphomas.
“There, too, we were able to detect CXCR5 on all B-lymphoma cells and follicular T helper cells,” Pfeilschifter said.
When she and Bunse placed the tumor cells in the petri dish together with the CXCR5-targeted CAR T cells, almost all of the malignant B and T helper cells disappeared from the tissue sample after 48 hours. The researchers then tested the new procedure on two mouse models. One model consisted of immune-suppressed animals that could be treated with human CAR T cells without causing rejection reactions. The researchers discovered no serious side effects in the mice.
“We also developed a pure mouse model for CLL specifically for the current study. We administered mouse CAR T cells against CXCR5 to these animals by infusion and were able to eliminate mature B cells and T helper cells, including malignant ones, from the B-cell follicles of the lymphoid organs,” reported Bunse.
For Höpken, the study is the first step toward creating a “living drug” — similar to other cellular immunotherapies being developed at the MDC.
“No laboratory can tackle such a study on its own. It has only come about thanks to a successful collaboration between many colleagues at the MDC and Charite,” stated Höpken.
“We are already cooperating with two cancer specialists at Charite, and are currently working with them to prepare a Phase 1/2 clinical trial,” added Rehm, who is a corresponding author of the study.
Höpken and Rehm hope that the first patients will begin to benefit from their new CAR-T cell therapy in the near future.

